In the ever-evolving landscape of American politics, few alliances have proved as surprising — and potentially consequential — as the connection between former President Donald Trump and celebrity physician Dr. Mehmet Oz. As the nation grapples with critical issues in healthcare, particularly Medicare and Medicaid, this unexpected partnership has sparked intrigue and speculation about its implications for millions of Americans. As the conversation around health policy intensifies, the Trump-Oz connection raises questions not only about leadership and influence but also about the future direction of healthcare initiatives in a nation seeking balance between accessibility and sustainability. In this article, we will explore the dynamics of their collaboration, assess its impact on healthcare reform discussions, and consider what it may mean for the future of Medicare and Medicaid in an era marked by change and uncertainty.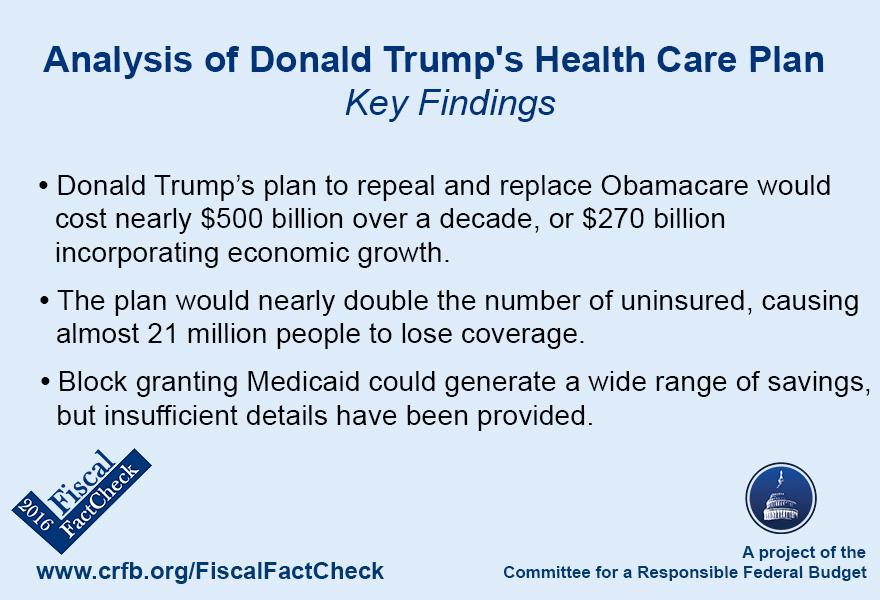
The Political Landscape of Healthcare Reform Under Trump and Oz
The political landscape surrounding healthcare reform has undergone significant change, particularly as the Trump administration intensified its focus on consumer-driven policies. With Donald Trump promoting the notion of competition as a key to improving healthcare access and affordability, initiatives like the expansion of Health Savings Accounts (HSAs) gained momentum. This approach fundamentally reshaped the discourse around Medicare and Medicaid, leading to a renewed emphasis on privatization and market solutions. Trump’s leadership encouraged states to explore waiver options, allowing for more flexibility in managing Medicaid programs, often spurring debates on the balance between federal oversight and state autonomy.
As Dr. Mehmet Oz stepped onto the political stage, he introduced another layer to this evolving narrative. His perceived connection to Trump amplified calls for innovative healthcare reforms that combined the celebrity appeal with grassroots understanding. Advocates for reform point out several key shifts that could define this era:
- Streamlined Access: Simplifying the enrollment process for Medicare and Medicaid could enhance accessibility.
- Telehealth Expansion: Proposals to sustain expanded telehealth services resonate with both rural and urban populations.
- Preventive Care Investments: There’s a growing focus on funding preventive care, aimed at reducing long-term costs.
| Aspect | Trump Era | Oz Influence |
|---|---|---|
| Medicaid Waivers | Increased state flexibility | Pushed for reform transparency |
| Consumer Choice | Enhanced market competition | Advocated for innovative therapies |
| Public Awareness | Limited outreach initiatives | Focused on community engagement |
As the legacy of the Trump administration continues to shape policy discussions, the interplay between his strategies and Oz’s vision remains to be seen. Their combined influence could usher in a new paradigm for healthcare, with the potential to address long-standing inefficiencies and inequities. The intersection of celebrity and politics may well catalyze a mobilization around healthcare issues that resonates with the broader public, prompting critical conversations about the future of Medicare and Medicaid within the American landscape.
Understanding the Implications for Medicare: A Shift in Priorities
The recent political shifts have ignited discussions about the future of Medicare, raising questions about what to expect from a potential transition in leadership. As the Trump-Oz connection gains traction, it opens the door to new priorities and policies that may significantly alter the landscape of healthcare for millions of Americans. Stakeholders are keenly watching how proposed changes could lead to a reallocation of resources, addressing existing gaps in service provision and potentially shaping the benefits structure. Key implications to consider include:
- Funding Adjustments: Shifting allocations may emphasize preventative care over emergency services.
- Policy Overhaul: Possible introduction of block grants for states, altering the financial framework of Medicaid.
- Access Disparities: Concerns over whether marginalized communities will continue to have adequate access to services.
- Innovation Incentives: Potential increase in funding for telehealth services and technological advancements.
Moreover, understanding the implications of these shifts necessitates a closer examination of how proposed policies will affect beneficiaries on the ground. A comparative analysis of projected changes in services and benefits can illuminate the potential outcomes of this new direction. The table below summarizes key aspects of the current system versus proposed changes:
| Aspect | Current System | Proposed Change |
|---|---|---|
| Funding Model | Fee-for-service | Value-based reimbursement |
| Focus Area | Reactive care | Preventative health |
| Medicaid Expansion | State-based decision | Uniform federal support |
| Technology Adoption | Limited telehealth | Increased access and reimbursement |
This evolving scenario invites critical scrutiny as stakeholders evaluate how these transformations align with the needs of the population they serve and the long-term sustainability of healthcare funding mechanisms. It remains to be seen whether these proposed changes will adequately address the needs of Medicare and Medicaid recipients, but careful observation and empirical evidence will be crucial in navigating this new frontier.
Medicaid Expansion and Accessibility: Potential Changes Ahead
As the political landscape shifts, discussions around Medicaid expansion and its impact on accessibility are increasingly taking center stage. The potential changes in this area could significantly alter the way millions of Americans interact with healthcare services. Advocates for expansion argue that broadening access is essential for ensuring that vulnerable populations receive the support they need. By expanding eligibility, states could witness a decrease in uninsured rates, leading to improved overall public health outcomes.
In this evolving dialogue, several factors must be considered moving forward. For instance, the relationship between federal funding and state autonomy raises important questions. The following points summarize some of the key considerations being discussed:
- Funding Challenges: How will changes in federal support impact state budgets?
- Health Equity: Will expansions truly reach underserved communities?
- Regulatory Shifts: What will be the impact of new guidelines on existing programs?
- Political Implications: How might local elections shape state-level decisions on Medicaid?
To further illustrate the potential effects on accessibility, consider the following table outlining hypothetical changes in enrollment numbers under an expanded Medicaid program:
| State | Current Enrollment | Projected Growth with Expansion |
|---|---|---|
| State A | 250,000 | 320,000 |
| State B | 100,000 | 170,000 |
| State C | 500,000 | 600,000 |
As these discussions unfold, the outcome of Medicaid expansion efforts remains to be seen, highlighting the need for informed dialogue and creative solutions. The resulting changes could redefine healthcare access for millions, presenting both opportunities and challenges in the quest for equitable health solutions.
Strategies for Advocating Patient-Centric Policies in a New Administration
As the political landscape shifts with a new administration, advocating for patient-centric policies becomes ever more critical. Stakeholders, including healthcare providers, patient advocacy groups, and community organizations, must collaborate to ensure that the needs of patients remain at the forefront of policy discussions. Key strategies to achieve this include:
- Building Coalitions: Engage diverse groups who share a common goal of improving patient outcomes to amplify the voice of the patient.
- Utilizing Data: Leverage healthcare data and case studies to present compelling narratives that highlight patient experiences and outcomes, making the case for policy changes.
- Participating in Public Forums: Attend town halls, hearings, and public discussions to raise awareness and express support for patient-focused initiatives.
Moreover, it’s essential to communicate the economic benefits of patient-centric policies, as cost-effective care models not only enhance patient satisfaction but also reduce overall healthcare spending. Advocates should consider:
| Benefit | Impact |
|---|---|
| Reduced Hospital Readmissions | Lower costs for both patients and insurers |
| Improved Chronic Disease Management | Increased quality of life and productivity |
| Enhanced Patient Satisfaction | Stronger patient-provider relationships leading to better adherence to treatment |
Creating a unified message around these strategies can significantly influence the new administration’s approach to Medicare and Medicaid, ensuring that patient voices are heard and valued in the policymaking process.
Q&A
Q&A: The Trump-Oz Connection: A New Era for Medicare and Medicaid? Q1: What does the term “Trump-Oz Connection” refer to in the context of Medicare and Medicaid? A1: The ”Trump-Oz Connection” refers to the potential influence that Donald Trump and Dr. Mehmet Oz might wield in shaping the future of Medicare and Medicaid policy. With Trump’s prominence in Republican politics and Oz’s recent foray into political office, their partnership could signal new strategies and reforms for these vital healthcare programs.
Q2: How might Trump and Oz’s shared vision impact healthcare policy? A2: Both Trump and Oz have been vocal on issues surrounding healthcare. Their collaboration could lead to a focus on conservative reforms, including expanded private sector involvement in Medicare and Medicaid, streamlining processes, and possibly altering eligibility criteria. Their approaches may also emphasize deregulation and the reduction of government oversight, which could significantly reshape these programs.
Q3: What are the potential benefits of a Trump-Oz influenced Medicare and Medicaid? A3: Proponents argue that a Trump-Oz influence could lead to innovative solutions aimed at cutting costs and improving patient outcomes. They might advocate for enhanced telehealth services, promote competition among healthcare providers, and analyze new payment models that reward efficiency and quality of care. Supporters believe these changes could make healthcare more accessible while maintaining or improving quality.
Q4: What criticisms are associated with this connection? A4: Critics voice concerns that increased privatization could undermine the foundational aspects of Medicare and Medicaid, making it difficult for low-income and elderly populations to access necessary care. They worry that profit-driven motives could overshadow the imperative to provide comprehensive healthcare services, potentially leading to reduced coverage and higher out-of-pocket costs for vulnerable populations.
Q5: How does the public perceive the relationship between Trump and Oz regarding healthcare? A5: Public opinion on the Trump-Oz relationship is polarized. Some view it as a positive shift toward responsible healthcare reform, while others see it as a further step away from equitable access to healthcare. Polling data suggests that the perceptions may vary significantly along partisan lines, with many Republicans supporting the connection, and a majority of Democrats expressing skepticism or concern.
Q6: What should stakeholders in healthcare, such as providers and patients, keep an eye on? A6: Stakeholders should closely monitor any proposed legislation that emerges from the Trump-Oz partnership. This includes being vigilant about changes in funding, eligibility requirements, and benefits within Medicare and Medicaid. Additionally, the implementation of any innovative programs or pilot projects should be scrutinized to assess their effectiveness and impact on patient care and access.
Q7: What could be the long-term implications of the Trump-Oz connection for Medicare and Medicaid? A7: The long-term implications could range from a complete overhaul of how these programs operate to a more modest recalibration of existing policies. Depending on political support and public reception, this collaboration could either solidify a new paradigm for health services in the U.S. or provoke significant backlash leading to calls for a return to previous policies. As healthcare remains a contentious issue, the evolving dynamics of the Trump-Oz connection are sure to influence the discussion for years to come.
Insights and Conclusions
As the political landscape continues to evolve, the unfolding dynamics between Donald Trump and Dr. Mehmet Oz represent more than just a partnership; they symbolize a potential shift in the national conversation around healthcare, particularly Medicare and Medicaid. As we reflect on their intertwined narratives, it becomes clear that the future of these crucial programs could be shaped significantly by the ideologies they advocate—a blend of populism, personal health narratives, and policy reform. The implications of this connection stretch far beyond the boundaries of party lines, inviting a deeper discussion about the accessibility, sustainability, and quality of care Americans deserve. Whether through innovative reforms or rekindled debates on longstanding issues, the engagement of influential figures like Trump and Oz will inevitably pose questions that warrant our attention. As we stand at this crossroads, it’s essential for citizens and policymakers alike to scrutinize the proposed changes and voice their perspectives, ensuring that the conversation remains inclusive and constructive. The coming months may well usher in a new era for Medicare and Medicaid—one that reflects not only the ambitions of its proponents but also the needs and values of the people it serves. As we turn the page, let us remain vigilant and engaged, striving to shape a healthcare system that prioritizes the well-being of all Americans.